Routine Blood work up at Dublin Health Screen to include renal function, liver function and inflammatory markers
Blood can be tested for many different things. The person who requests the blood test will write on the form which tests they want the ‘lab’ to do. Different blood bottles are used for different tests. For example, for some tests the blood needs to clot and the test is looking for something in serum. For some tests, the blood is added to some chemicals to prevent it from clotting. If the blood glucose is being measured, then the blood is added to a special preservative, etc. This is why you may see your blood added to blood bottles of different sizes and colours. In the case of a health screen then the largest range of bloods possible are taken.
Blood tests are taken for many different reasons, for example, to:
- Help diagnose certain conditions, or to rule them out if symptoms suggest possible conditions.
- Monitor the activity and severity of certain conditions. For example, a blood test may help to see if a condition is responding to treatment.
- Check the body’s functions such as liver and kidney function when you are taking certain medicines which may cause side-effects.
- Check your blood group before receiving a blood transfusion.
The standard blood tests at Dublin health screen are as follows,
- Full blood count – checks for anaemia, and other conditions which affect the blood cells.
- Blood chemistry.
- Kidney function.
- Liver function.
- Hormone levels.
- Blood glucose (sugar) level.
- Tests for inflammation.
- Blood cholesterol level.
- To check the levels of certain medicines to ensure you are taking the correct dose.
- Immunology – such as checking for antibodies to certain viruses and bacteria.
What is normal blood made up of?
Blood cells, which can be seen under a microscope, make up about 40% of the blood’s volume. Blood cells are divided into three main types:
-
- Red cells (erythrocytes). These make blood a red colour. One drop of blood contains about five million red cells. A constant new supply of red blood cells is needed to replace old cells that break down. Millions of red blood cells are made each day. Red cells contain a chemical called haemoglobin. This binds to oxygen, and takes oxygen from the lungs to all parts of the body.
- White cells (leucocytes). There are different types of white cells which are called neutrophils (polymorphs), lymphocytes, eosinophils, monocytes, and basophils. They are part of the immune system. Their main role is to defend the body against infection.
- Platelets. These are tiny and help the blood to clot if we cut ourselves.
- Plasma is the liquid part of blood and makes up about 60% of the blood’s volume. Plasma is mainly made from water, but also contains many different proteins and other chemicals such as hormones, antibodies, enzymes, glucose, fat particles, salts, etc.
When blood spills from your body (or a blood sample is taken into a plain glass tube) the cells and certain plasma proteins clump together to form a clot. The remaining clear fluid is called serum.
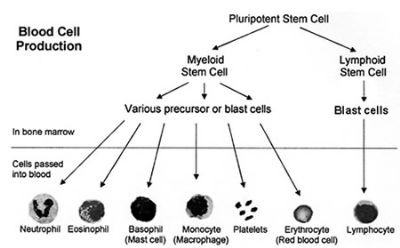
Bone marrow
Blood cells are made in the bone marrow by ‘stem’ cells. The bone marrow is the soft ‘spongy’ material in the centre of bones. The large flat bones such as the pelvis and breast-bone (sternum) contain the most bone marrow. To constantly make blood cells you need a healthy bone marrow. You also need nutrients from your diet including iron and certain vitamins.
Stem cells
Stem cells are primitive (immature) cells. There are two main types in the bone marrow – myeloid and lymphoid stem cells. These derive from even more primitive common ‘pleuripotent’ stem cells. Stem cells constantly divide and produce new cells. Some new cells remain as stem cells and others go through a series of maturing stages (‘precursor’ or ‘blast’ cells) before forming into mature blood cells. Mature blood cells are released from the bone marrow into the bloodstream.
- Lymphocyte white blood cells develop from lymphoid stem cells. There are three types of mature lymphocytes:
- B lymphocytes make antibodies which attack infecting bacteria, viruses, etc.
- T lymphocytes help the B lymphocytes to make antibodies.
- Natural killer cells which also help to protect against infection.
- All the other different blood cells (red blood cells, platelets, neutrophils, basophils, eosinophils and monocytes) develop from myeloid stem cells.
Blood production
You make millions of blood cells every day. Each type of cell has an expected life-span. For example, red blood cells normally last about 120 days. Some white blood cells last just hours or days – some last longer. Every day millions of blood cells die and are broken down at the end of their life-span. There is normally a fine balance between the number of blood cells that you make, and the number that die and are broken down. Various factors help to maintain this balance. For example, certain hormones in the bloodstream, and chemicals in the bone marrow called ‘growth factors’, help to regulate the number of blood cells that are made.
What is a blood group?
Red blood cells have certain proteins on their surface called antigens. Also, your plasma contains antibodies which will attack certain antigens if they are present. There are various types of red blood cell antigens – the ABO and rhesus types are the most important.
ABO types
These were the first type discovered.
- If you have type A antigens on the surface of your red blood cells, you also have anti-B antibodies in your plasma.
- If you have type B antigens on the surface of your red blood cells, you also have anti-A antibodies in your plasma.
- If you have type A and type B antigens on the surface of your red blood cells, you do not have antibodies to A or B antigens in your plasma.
- If you have neither type A or type B antigens on the surface of your red blood cells, you have anti-A and anti-B antibodies in your plasma.
Rhesus types
Most people are ‘rhesus positive’ as they have rhesus antigens on their red blood cells. But, about 3 in 20 people do not have rhesus antibodies and are said to be ‘rhesus negative’.
Blood group names
Your ‘blood group’ depends on which antigens occur on the surface of your red blood cells. Your blood group is said to be:
- A+ (A positive) if you have A and rhesus antigens.
- A– (A negative) if you have A antigens, but not rhesus antigens.
- B+ (B positive) if you have B and rhesus antigens.
- B– (B negative) if you have B antigens, but not rhesus antigens.
- AB+ (AB positive) if you have A, B and rhesus antigens.
- AB– (AB negative) if you have A and B antigens, but not rhesus antigens.
- O+ (O positive) if you have neither A nor B antigens, but you have rhesus antigens.
- O– (O negative) if you have do not have A, B or rhesus antigens.
Other blood types
There are many other types of antigen which may occur on the surface of red blood cells. However, most are classed as ‘minor’ and are not as important as ABO and rhesus.
How does blood clot?
Within seconds of cutting a blood vessel, the damaged tissue causes platelets to become ‘sticky’ and clump together around the cut. These ‘activated’ platelets and the damaged tissue release chemicals which react with other chemicals and proteins in the plasma called ‘clotting factors’. There are 13 known clotting factors which are called by their Roman numbers – factor I to factor XIII. A complex cascade of chemical reactions involving these clotting factors quickly occurs next to a cut. The final step of this cascade of chemical reactions is to convert factor I (also called fibrinogen – a soluble protein) into thin strands of a solid protein called fibrin. The strands of fibrin form a meshwork, and trap blood cells and platelets so that a solid clot is formed.
If a blood clot forms within a healthy blood vessel it can cause serious problems. So, there are also chemicals in the blood which prevent clots from forming, and chemicals which ‘dissolve’ clots. So, there is a balance between forming clots and preventing clots. Normally, unless a blood vessel is damaged or cut, the ‘balance’ tips in favour of preventing clots forming within blood vessels.
Some types of blood disorders
Problems with blood cells
- Anaemia means that you have less red blood cells than normal, or have less haemoglobin than normal in each red blood cell. There are many causes of anaemia. For example, the most common cause of anaemia in the UK is a lack of iron. (Iron is needed to make haemoglobin.) Other causes include lack of vitamins B12 or folate which are needed to make red blood cells. Abnormalities of red blood cell production can cause anaemia. For example, various hereditary conditions such as sickle cell disease and thalassaemia.
- Too many red cells is called polycythaemia and can be due to various causes.
- Too few white cells is called leucopenia. Depending on which type of white cell is reduced it can be called neutropenia, lymphopenia, or eosinopenia. There are various causes.
- Too many white blood cells is called leucocytosis. Depending on which type of white cell is increased it is called neutrophilia, lymphocytosis, eosinophilia, monocytosis, basophilia. There are various causes. For example:
- various infections can cause an increase of white blood cells.
- certain allergies can cause an eosinophilia.
- leukaemia causes a large increase in the number of white blood cells. The type of leukaemia depends on the type of white cell affected.
- Too few platelets which is called thrombocytopenia. This may make you bruise or bleed easily. There are various causes.
- Too many platelets which is called thrombocythaemia. This is due to disorders which affect cells in the bone marrow which make platelets.
Bleeding disorders
There are various conditions where you tend to bleed excessively if you damage or cut a blood vessel. For example:
- Too few platelets (thrombocytopenia) – due to various causes.
- Genetic conditions where you do not make one or more clotting factors. The most well known is haemophilia A which occurs in people who do not make factor VIII.
- Lack of vitamin K can cause bleeding problems as you need this vitamin to make certain clotting factors.
- Liver disorders can sometimes cause bleeding problems as your liver makes most of the clotting factors.
Clotting disorders
Sometimes a blood clot forms within a blood vessel which has not been injured or cut. For example:
- A blood clot which forms within a coronary (heart) artery or in an artery within the brain is the common cause of heart attack and stroke. The platelets become sticky and clump next to patches of atheroma (fatty material) in blood vessels and activate the clotting mechanism.
- Sluggish blood flow can make blood clot more readily than usual. This is a factor in deep vein thrombosis (DVT) which is a blood clot that sometimes forms in a leg vein.
- Certain genetic conditions can make the blood clot more easily than usual.
- Certain medicines can affect the blood clotting mechanism, or increase the amount of some clotting factors, which may result in the blood clotting more readily.
- Liver disorders can sometimes cause clotting problems as your liver makes some of the chemicals involved in preventing and dissolving clots.