At Dublin Health Screening
What is a cholesterol test?
A cholesterol test is a blood test that measures your total blood cholesterol level and its components, which include:

- high-density lipoprotein (HDL) cholesterol – ‘good cholesterol’
- low-density lipoprotein (LDL) cholesterol – ‘bad cholesterol’
- triglycerides
- total cholesterol
- total cholesterol/HDL ratio.
Together, the results are known as your blood lipid profile. Lipids are just another name for the fatty substances in the body and bloodstream. Note we ask you to fast for 12 hours before hand, having no breakfast, you also have to avoid tea and coffee but you can drink as much water as you want.
Why is it useful?
The cholesterol test is not used to diagnose a disease. Instead, measuring cholesterol and knowing the levels of these lipids provides important information on your health and your long-term risk of heart disease and stroke. Together with other cardiovascular risk factors (such as blood pressure, and bodyweight), your cholesterol results can give us an overall picture of your health.
If the blood test results are not within normal limits, this ‘early warning’ allows you to make lifestyle changes and consider treatments to lower your future risk of heart attack and stroke. Making changes on the advice of our doctors can greatly alter your risk.
How is it carried out?
Some cholesterol tests can be conducted with a finger-prick blood sample, but more detailed testing requires a blood sample collected from a vein in the arm. You will need to fast (go without food and most drink apart from water) for a specified period (usually at least 12 hours) before taking the test. You should still be allowed to drink water and take your normal medications – do not stop taking these unless your doctor advises you to (eg, if the medications would interfere with the test result).

Top 30 Cholesterol Lower Foods Dublin Health Screening
1 Oats and oat bran – Oats is a cholesterol buster. One of its component’s beta-glucan, helps in absorbing LDL (the bad cholesterol) which the body then excretes. According to the studies, as little as 3 grams of soluble oat fibre daily, present in one bowl of oatmeal, can reduce total cholesterol by 8-23 per cent in people who are suffering from high cholesterol issues.
2 Beans and legumes – Beans like kidney beans (rajma), bengal Gram (chana) and chick peas (kabuli chana), are rich in dietary fibre which help in reducing cholesterol level and thus, can prevent the rise of blood sugar levels.
3 Avocados – Rich in vitamin K, C, B5, B6, E, potassium and folate, along with a small quantity of magnesium, manganese, copper, iron, zinc, phosphorus, vitamin A, B1 (Thiamine), B2 (Riboflavin) and B3 (Niacin), protein, avocados are low-carb plant food. They keep a healthy blood pressure which is a solution for a lot of problems, one of them being cholesterol.
4 Nuts – Studies have shown that eating a whole walnut daily, for a month helps in lowering cholesterol by 5.4 per cent and LDL cholesterol by 9.3 per cent. Almonds and cashews are other good options for treating cholesterol.
5 Barley and other grains – Like oats, barley and other whole grains lower the risk of heart diseases, because of the soluble fibre they deliver. Barley also controls triglyceride level and regulates blood sugar level.
6 Eggplant and okra – These two low-calorie vegetables are good sources of soluble fibre and fibre is essential to control cholesterol level in the body.
7 Fruits – Fruits are a boundless source of nutrients, vitamins, minerals and fibre. Fruits such as pear, apples, oranges, berries, grapefruit and pomegranate have the necessary nutrients and components that aid in reducing the cholesterol level in the blood. It is also because their high fibre content help in reducing cholesterol level.
8 Soy – Soy, also known as soyabeans, have the ability to improve the metabolism, help gain healthy weight, protect heart, defend against cancer. It also reduces the effect of menopause, improves digestive health, promotes bone health, protects against birth defects, increases circulation and decreases the risk of diabetes. Its products like tofu, nuggets, Nutella, soy nuts and unflavoured soy milk help to lower cholesterol levels in the blood. It is a great substitute of the animal protein for the vegetarians as it lowers the level of total cholesterol, bad LDL cholesterol, and triglycerides without lowering HDL (good) cholesterol levels.
9 Fatty Fish – Fish is high in omega-3 fatty acids and protein. The omega-3 fatty acid in fish when consumed, reduces the triglyceride level by as much as 25-30 per cent while increasing the level of high-density lipoproteins (HDL) that are good for heart health.
10 Olive oil – Vegetable oils are also beneficial and useful in lowering cholesterol levels in the body. Using oils such as sunflower and other varieties, in place of butter in cooking or at the table help in lowering LDL.
11 Rice bran oil – With the balance of polyunsaturated fats (PUFA) and monounsaturated fats (MUFA), rice bran oil is one of healthiest cooking oils. As it contains the right amount of oryzanol, which is an antioxidant, rice bran oil thus decreases cholesterol absorption and increases our body’s ability to eliminate excess cholesterol.
12 Tomatoes – Rich in vitamins and minerals, tomatoes are good for hydration, to stimulate blood circulation, increase red blood cells and platelets and even fight against different forms of cancer. It detoxifies the body, reduces cholesterol, increases digestion, improves eyesight and provides relief from various skin problems.
13 Fenugreek seeds – Fenugreek seeds, or more commonly known as Methi seeds, have the ability to lower total cholesterol, LDL (bad cholesterol) and triglyceride level in the blood. According to the studies conducted, it is seen that the regular consumption of fenugreek seeds are also effective in controlling blood sugar level in people with diabetes.
14 Lemons – Lemon juice is a great way to consume vitamin C every day. Drinking lemon juice daily reduces the level of LDL, or “bad,” cholesterol in the body. Lemon Juice is one of the best natural cleansers because of its high citric acid content. The best time to drink lemon juice is in the morning, just after getting out of the bed. Drinking lemon juice on an empty stomach every day keeps your body healthy and free of impurities.
15 Ginger – Ginger is the best solution for healthy stimulation and increases blood circulation. While during winter, it keeps us warm and helps in getting rid of throat infections. Ginger is also rich in good enzymes and natural oil which reduces the level of bad cholesterol from the body.
16 Garlic – As garlic is known for its antibiotic properties, it should be mixed with food after chopping or crushing for better absorption of its nutrients.
17 Ispaghula husk – Also known as Psyllium, Ispaghula husk is a dietary fibre mainly consumed to get relief from the symptoms of both constipation and mild diarrhoea. It is also sometimes used as a food thickener. Studies have shown that ispaghula benefits in reducing blood cholesterol level.
18 Green Tea – Green Tea is one thing that can be found in almost every household and is a natural medicine to aid digestion. It also improves heart and mental health and regulates body temperature.
19 Coriander – Coriander seeds are very useful in lowering the cholesterol level. The best way to consume coriander is by boiling two tablespoons of coriander seeds in a glass of water, strain the decoction after cooling and drink it twice a day for effective results.
20 Cluster beans – Cluster beans, also known as Guar beans, which are a rich source of dietary fibre (guar gum). It is beneficial in lowering cholesterol level.
21 Cinnamon – Even half a teaspoon of cinnamon a day significantly reduces the blood sugar level, triglycerides and LDL (bad) cholesterol in people suffering from type 2 diabetes
22 Celery – Celery has a high antioxidant content and thus, it is known to lower the risk of heart disease by preventing oxidation of LDL (bad) cholesterol.
23 Broccoli and other vegetables – Broccoli contains cholesterol-lowering properties. The fibre in broccoli lowers cholesterol by binding with bile acids in the digestive tract and excreting it out of the body.
24 Apple cider vinegar – Apple cider vinegar is an excellent health tonic promoted for treating allergies, rashes, and infections and for aiding digestion and promoting weight loss. Vinegar maintains the pH level in the body and has a rich amount of potassium and enzymes which also helps in making a healthier body.
25 Brown Rice – Brown rice is the unpolished form of rice that retains most of its fibre and nutrient content that is otherwise removed from refined, white or polished rice. The brown rice is rich in nutrients including B vitamins, selenium, magnesium and phytonutrients.
26. Red Wine.
27 Dark Chocolate
28 Flax Seeds
29. Foods with added sterols and stanols, Flora Proactive spreads and drinks and the Benecol range.
30. Cut all Salt out of the diet and avoid processed food with salt, eg soup and bread.
Dr John J Ryan
Chlamydia in Women and Men screen, an optional test only depending on clinical risk

Chlamydia is the most common sexually transmitted infection in Ireland. It often causes no symptoms, and can be passed on to others without you realising. However, symptoms and complications may develop if it is left untreated. A short course of an antibiotic clears the infection in most cases.
What is chlamydia?
Chlamydia is an infection caused by a bacterium (germ) called Chlamydia trachomatis. In women, chlamydial infection usually affects the cervix and uterus (the womb). In men, it usually affects the urethra in the penis.
How do you get chlamydia and how common is it?
Most people with chlamydia got the infection by having sex with an infected person. About 1 in 20 sexually active women in Ireland are infected with chlamydia. It is most common in women under 25. (About 1 in 12 women aged 20 are infected with chlamydia.) The number of cases has risen sharply in recent years. Many women are not aware that they are infected as it often causes no symptoms. You can be infected with chlamydia for months, even years, without realising it.
The risk of infection increases with the number of changes of sexual partner. Wearing a condom during sex helps to prevent chlamydia and other sexually transmitted infections.
What are the common symptoms of chlamydia?
No symptoms occur in up to 8 in 10 cases. If symptoms do occur, they can include:
- Vaginal discharge. This is due to the cervix becoming inflamed.
- Pain or burning when you pass urine.
- Bleeding or spotting between periods. In particular, bleeding after you have sex.
- Pain or discomfort in the lower abdomen (pelvic area), especially when you have sex.
Why should I have treatment if I have no symptoms?
- Because the infection may spread and cause serious complications (see below). This can be months or years after you are first infected.
- You can pass on the infection to your sexual partner(s) even if you do not have symptoms.
Do I need any tests?
Chlamydia can be confirmed by a ‘swab’ taken from the cervix and urethra. (A swab is a small ball of cotton wool on the end of a stick which is used to obtain mucus and cells to send to the lab for testing.) Newer tests using a urine sample or a swab from the lower vagina are becoming increasingly used. You may also be advised to be tested for other sexually transmitted infections.
What is the treatment for chlamydia?
A short course of an antibiotic usually clears chlamydial infection. Even if you have no symptoms, treatment is strongly advised to prevent possible complications. Tell your doctor if you are (or may be) pregnant. This may affect the choice of antibiotic. Do not have sex until you and your sexual partner have finished treatment (or for seven days after treatment with a ‘single dose’ antibiotic which is sometimes used).
Does my partner need to be treated?
Yes. Also, any other sexual partners within the past six months should also be tested for infection. (If you have not had sex within the last six months then your latest sexual partner should be tested and treated, however long ago the relationship was.) A course of an antibiotic is usually advised whether or not infection is found on testing. This is because:
- Chlamydial infection is commonly passed on during sex.
- Men and women often have no symptoms with chlamydia, but can still pass on the infection.
- The test for chlamydia is not 100% reliable. Treatment makes sure that any possible infection which may have been missed by the tests is cleared.
- If your sexual partner is infected and not treated, chlamydia can be passed back to you again after you are treated.
What are the possible complications of chlamydia?
- If left untreated, the infection may seriously affect the uterus and fallopian tubes (called ‘pelvic inflammatory disease’ or PID). About 1 in 5 women with chlamydia develop PID. This may develop suddenly and cause fever and pain. It can also develop slowly over months or years without causing symptoms (also known as ‘silent PID’). However, over time, scarring or damage to the fallopian tubes may occur and can cause:
- Chronic (persistent) pain.
- Difficulty becoming pregnant (infertility).
- If you become pregnant, you have an increased risk of ectopic pregnancy (where the pregnancy develops in a fallopian tube and can cause serious life-threatening problems). About 4 in 10 ectopic pregnancies are due to infection with chlamydia.
- The risk of developing some complications of pregnancy such as miscarriage, premature birth, and stillbirth are increased in pregnant women with untreated chlamydia.
- If you have untreated chlamydia during childbirth, your baby may develop a chlamydial infection of their eye or lung during the birth.
- Reiter’s syndrome is a rare complication. This causes arthritis and eye inflammation. It may be due to the immune system ‘over-reacting’ to chlamydial infection in some cases.
The risk of complications is much reduced if chlamydial infection is treated early.
What causes non-gonococcal urethritis?
- Infection with chlamydia causes about half of cases of NGU. Chlamydia is a bacterium (germ) that is usually caught by sexual contact with an infected person. You can pass chlamydia on during vaginal, anal or oral sex.
- Various other bacteria or viruses which are sexually transmitted can cause NGU.
- A non-infective problem is, rarely, the cause. For example, injury or surgery to the urethra can cause inflammation.
- No cause can be found in about 1 in 4 cases. Sexually transmitted infections that are not identified by tests are probably the cause of some of these, but not all. However, it is not possible to say which of these cases are due to infection and which are not.
What are the symptoms of non-gonococcal urethritis?
- A white discharge (fluid) from the end of the penis is common, but does not occur in every case.
- Pain or burning when you pass urine. This may be confused with a urine infection.
- Irritation inside the penis.
- A feeling of wanting to pass urine frequently.
- In a small number of cases the infection travels up the urethra to the testes and causes pain and swelling in one or both testes.
- A rare complication is a type of arthritis which can be triggered by NGU. It may be due to the immune system ‘over-reacting’ to some bacteria that can cause NGU.
- Up to half of men with chlamydia infection (the most common cause of NGU) do not have any symptoms.
The symptoms may clear over time, even without treatment. This may take up to six months, but can be just a couple of weeks or so. However, without treatment, bacteria that cause NGU often remain in the urethra. It is just that the symptoms may go.
Therefore, even if symptoms go, there is a good chance that you can pass on the infection if you are not treated.
A specimen of the discharge (a ‘swab’), and/or a urine specimen, may be taken to try and identify the cause of the infection. You may also be advised to have tests for other sexually transmitted infections.
What is the treatment for non-gonococcal urethritis?
A short course of antibiotics usually clears NGU. The antibiotic prescribed may depend on which bacteria are found (often chlamydia), and whether other infections are also present.
If no bacteria are found by the tests, you may still be advised to take a course of antibiotics if you have symptoms of NGU. Infection is still the likely cause, even if a bacterium cannot be identified.
Most people get better with antibiotic treatment.
Follow-up
A doctor or health care professional will often want to know that treatment has worked. It is common to be reviewed a couple of weeks after you start treatment to check that symptoms have gone. Sometimes re-testing and a second antibiotic is needed if symptoms persist.
You should not have sex until both you and your sexual partner(s) have finished treatment.
About Haemochromatosis a simple blood test at Dublin Health Screening
 Haemochromatosis, or GH (Genetic Haemochromatosis), is a genetic disorder causing the body to absorb an excessive amount of iron from the diet: the iron is then deposited in various organs, mainly the liver, but also the pancreas, heart, endocrine glands, and joints.
Haemochromatosis, or GH (Genetic Haemochromatosis), is a genetic disorder causing the body to absorb an excessive amount of iron from the diet: the iron is then deposited in various organs, mainly the liver, but also the pancreas, heart, endocrine glands, and joints.
Normally the liver stores a small amount of iron for the essential purpose of providing new red blood cells with iron, vital for health. When excessive quantities of iron are stored in the liver it becomes enlarged and damaged. Deposits of iron may also occur in other organs and joints, causing serious tissue damage.
For a long time it was believed that the disorder was rare, so GH was seldom considered as a possible diagnosis. However, recent surveys of people of Northern European origin have shown a prevalence of 1 in 400 likely to be at risk of developing iron overload. GH is now recognised as being one of the most common genetic disorders.
Symptoms
- Chronic fatigue, weakness, lethargy.
- Abdominal pain; sometimes in the stomach region or the upper right-hand side, sometimes diffuse.
- Arthritis; may affect any joint but particularly common in the knuckle and first joint of the first two fingers. The bronze fist (diagram right) – is an arthritic symptom typical of hemochromatosis.
- Diabetes (late onset type).
- Liver disorders; abnormal liver function tests, enlarged liver, cirrhosis.
- Sexual disorders; loss of sex drive, impotence in men, absent or scanty menstrual periods and early menopause in women, decrease in body hair.
- Cardiomyopathy; disease of the heart muscle (not to be confused with disease of the arteries of the heart).
- Neurological/psychiatric disorders; impaired memory, mood swings, irritability, depression.
- Bronzing of the skin, or a permanent tan.
Most of these symptoms are found in other disorders. Chronic fatigue may be ascribed to the after-effects of a viral infection or to psychological causes, and abdominal pain to irritable bowel syndrome. Similarly, liver disorders may be put down to excessive alcohol intake, even in someone who is only a moderate drinker. However, if the above symptoms are present, GH should also be considered as a diagnosis.
Most individuals who have GH will, in due course, develop at least one or two of the above symptoms, although possibly in a very mild form. There may be a long phase of the condition where there are no symptoms. However, if arthritis is found only in the first two finger joints this is highly suggestive of GH.
The need for treatment to remove excess iron does not depend upon the presence of clinical symptoms. The risk of developing a serious complaint such as cirrhosis is much too great to be overlooked.
How is it inherited?
Inherited disorders are caused by defective genes in the cells which make up the body. Genes, which are made of DNA, contain the information the body needs to develop from the egg and to maintain itself in good working order. There are about 30,000 genes and every cell in the body, except sperm and egg cells, contains two copies of each. One of these copies is inherited from the mother and one from the father.
In 1996 the HFE gene was identified as the major gene affected in haemochromatosis. A small change (mutation) is present in both copies of the gene in over 90% of those diagnosed with GH. GH is a ‘recessive’ disorder. The risk of absorbing excess iron will only occur if both copies of the gene are abnormal. If only one copy is defective, an individual will be perfectly healthy but will be a ‘carrier’. This means he or she will be able to pass on the abnormal gene to a son or daughter.
Sperm and egg cells have only one copy of each gene, and on average half the eggs or half the sperm of a carrier will contain the defective version. By contrast, ALL the eggs or sperm of an individual in whom both gene copies are defective and who, as a result, suffers from GH, will carry the abnormal gene.
To develop GH you have to inherit a defective gene from both your parents. This can happen in three ways:
- If both parents are carriers (most common – about 10% of the population are carriers, so 1% of marriages will be between carriers). On average a quarter of the children will develop GH, half will be carriers, and a quarter will be normal.
- If one parent has GH and the other is a carrier (about 1 in 2000 marriages), on average half the children will develop GH, the other half will be carriers.
- If both parents suffer from GH, (a rare event, occurring in about 1 in 100,000 marriages) all the children will inherit two defective genes, and will have GH.
It should be emphasised that the proportions given in examples 1 and 2 are averages for the whole population: in any particular family where both parents are carriers (example 1) it would be possible for all children to be affected, all to be carriers, or for all to be normal.
Relatives who are at risk should be tested. This is absolutely essential in the case of brothers and sisters (siblings) as they stand at least a 1 in 4 chance of being affected. Parents, partners and children from the age of 18, should also be tested.
What are the tests?
- Serum Ferritin
This indicates the amount of iron stored in the body. Levels significantly over 300mcg/l [micrograms per litre] in men and 200æg/l in women are further evidence of GH. It should be realised that in the early stages of iron accumulation, serum ferritin may be within the normal range. Raised TS with a normal serum ferritin level does not rule out a diagnosis of GH.
2. Gene Test
A simple blood test for the HFE gene mutation is positive in over 90% of those affected. It will identify family members at risk of loading iron.
What is the treatment?
The simple and effective treatment consists of regular removal of blood. Known as venesection therapy or phlebotomy, the procedure is the same as for blood donors. Every pint of blood removed contains a quarter of a gram of iron. The body then uses some of the excess stored iron to make new red blood cells. Venesection will usually be performed once a week, depending on the degree of iron overload. Treatment may need to be continued at this frequency for up to 2 years, occasionally longer.
During the course of treatment, the serum ferritin levels are monitored, indicating the size of the remaining iron stores. Treatment should usually continue until the serum ferritin level reaches 20æg/l (indicating minimal or absent iron stores).
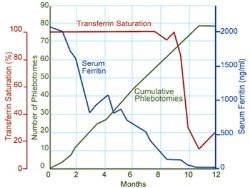
This is not the end of the story. Excess iron will continue to be absorbed so the individual will need occasional venesections (maintenance therapy), on average every 3 to 4 months, for the rest of his or her life. Monitoring of transferrin saturation and serum ferritin is used to assess whether venesection is required more or less often. The transferrin saturation should be maintained below 50% and the serum ferritin below 50mcg/l.
The graph on the right gives an example of how treatment may affect blood iron levels during treatment. Serum ferritin decreases steadily, but transferrin saturation remains high until iron deficiency occurrs, then falls sharply.
How effective is treatment?
Venesection treatment will cause tissue iron to be mobilised and iron stores will return to normal. However, it will not cure some serious clinical conditions such as diabetes or cirrhosis if they are already present at the time treatment is started. This emphasises the need for early diagnosis.
- Fatigue, lethargy and abdominal pain should decrease.
- Cardiomyopathy should improve providing cardiac damage is not severe. In severe cases iron chelation treatment can reverse congestive heart failure.
- Bronzing of the skin should fade.
- Cirrhosis will stay the same.
- Sexual dysfunction and arthritis do not usually improve. Indeed arthritis may appear later even if absent at the time of diagnosis and treatment.
- Providing there is not a massive, long-standing iron overload present at the time treatment is started; those who undergo treatment have a normal life expectancy.
What about diet?
It is not possible to treat GH with a low iron diet. A nutritional natural diet is recommended – the graph on the right illustrates the iron content of a sample of foods, ave
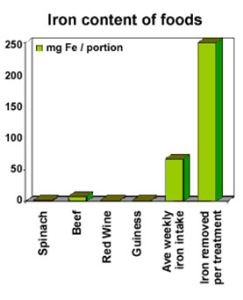
rage weekly intake and the amount of iron removed in each treatment. We make the following recommendations:
+ Avoid vitamin supplements or tonics containing iron, and breakfast cereals heavily fortified with iron. Large doses of vitamin C should also be avoided, as it makes the process of depositing iron in some organs easier and enhances the absorption of iron from the diet.
+ Reduce intake of offal (liver, kidney etc.) and red meat. The rate of iron absorption from red meat is 20 to 30% whereas vegetables and grains have less iron and a 1 to 20% rate of absorption.
+ Minimise alcohol intake, particularly with meals, as it may increase iron absorption and it can also cause liver disease. Tea and all milk products taken with a meal reduce the amount of iron
Osteoporosis is a condition in which the skeleton loses bone mass and minerals, and bones become more porous, thinner and weaker, leading to an increased risk of a fracture. Osteoporosis is on the increase in Ireland, partly due to the ageing population, but also to dietary and lifestyle influences. People usually equate osteoporosis with a poor intake of calcium, the menopause in women and older age. This is certainly true – but excess alcohol, protein malnutrition, smoking, some medications, lack of exercise and other lifestyle factors also impair bone health. We will arrange a Dexa Scan as needed through our local hospital systems.
Calcium
Calcium is a vital bone-building material – protecting against osteoporosis – but it cannot do its job without adequate vitamin D. Bone also provides the “calcium reservoir” for maintaining correct calcium levels in the blood. Milk and dairy foods are among the richest and most easily accessible sources of calcium – a 250ml glass of milk contains about 300mg calcium. Three servings of dairy foods a day usually ensures adequate calcium intake of around 1000mg per day. Other good sources are foods and beverages fortified with calcium, small fish with bones, nuts, tofu and certain vegetables (eg, broccoli).
In one vulnerable group – teenage girls – calcium intake fell well short of the recommended 1000mg, a recent Irish study showed. Many adults also did not consume two to three dairy servings a day and were probably not meeting the recommended intakes. Bone density and strength can be compromised later in life if there is inadequate calcium consumption, particularly during the growing years and early adulthood.
Vitamin D
Vitamin D occurs naturally in small amounts in some foods (see below) but diet is not the main source – vitamin D is mainly created through the action of sunlight on the skin. Most diets (without supplements) are not thought to provide sufficient vitamin D. An international study of over 2500 postmenopausal women who have osteoporosis has found most of these women are deficient in vitamin D. Vitamin D was first identified as being an essential nutrient when it was discovered children given cod liver oil (high in vitamin D) did not develop rickets (early age bone deformities). Later, it was found that exposure to sunlight had a similar effect (see below). And, even recently, an Irish study has reported that, while figures are no longer routinely kept, cases of rickets in children are still appearing. A vitamin D deficiency during pregnancy is believed to be an important cause (the infant also starts life with a deficiency), as is extreme protection of children from sunlight.
Vitamin D and calcium should be considered of equal importance for maintaining healthy bones throughout your entire life. Vitamin D has many functions but bone health is an important one.
- Vitamin D allows calcium absorption; without it your digestive system cannot absorb as much calcium from food.
- Vitamin D is needed for the proper mineralisation and growth of bone.
- Studies have shown that correction of vitamin D and calcium deficiencies in elderly women reduces fracture rates.
- Correction of vitamin D deficiency separately reduces body sway and the risk of falling in elderly women, perhaps by improving nerve-muscle function.
- Evidence increasing points to a role for vitamin D in the immune system and regulating blood pressure.
Foods containing vitamin D
- Fatty fish, eg, salmon, mackerel, sardines (rich source)
- Cod liver oil (rich source)
- Liver
- Some fortified foods (moderate source), eg:
-margarines
-milk
-dairy foods
-cereals.
Vitamin D: the “sunshine” vitamin
Vitamin D is often referred to as the sunshine vitamin – normally, 90% of our requirement comes from the action of sunlight (ultraviolet light; UV), which penetrates the skin and activates pre-vitamin D into vitamin D (through reactions in the skin, liver and kidneys). Vitamin D manufacture by the skin is normally much greater than the amounts obtained from food. Exactly how much vitamin D is obtained from the ultraviolet light in sunlight, and therefore how much sun exposure is needed each day, depends on:
- Skin pigmentation – darker skin needs more UV to produce vitamin D
- Season, time of day – the less intense the sun, the more is needed
- Duration of exposure to sunlight
- Coverage by clothing or sunscreen
- Whether sitting behind glass or plastic.
Consequently, those at risk for a vitamin D deficiency include:
- Darker skinned adults
- Dark-skinned children, particularly if they are also iron deficient
- People whose skin is largely always covered for religious reasons or custom (especially women and children)
- Vitamin D deficient pregnant women who may predispose newborns to vitamin D deficiency
- Infants entirely breastfed beyond six months without sunlight exposure or vitamin D supplementation
- Older adults who are seldom outside (eg, housebound or in residential care) and are not receiving vitamin D supplementation.
How much sun exposure is needed?
If the adequate sun exposure is not possible a daily vitamin D supplement of 400IU (10 micrograms) is recommended. Dark-skinned people will require more sun exposure than fair skinned people. Ultraviolet light is the radiation most commonly associated with sunburn and skin cancer.
Comments in medical journals in 2010 describe frank vitamin D deficiency in up to 8% of younger women at the end of winter and in 15% of dark-skinned pregnant women attending an antenatal clinic in Dublin. A similar proportion (17%) with deficiency was found in a study of 90 pregnant women of all backgrounds and ethnicities attending an antenatal health service check. Other researchers in Dublin found up to 46% of elderly people in nursing homes had very low levels of vitamin D. The elderly are most at risk of developing osteoporosis and having falls and fractures if adequate calcium and vitamin D are not maintained. Doctors are well aware of the osteoporosis risks and can help you identify whether you are at risk of a nutritional deficiency or developing osteoporosis. If you have a deficiency, supplementation of calcium and vitamin D may be recommended.
What Are Tumor Marker Tests for Cancer?
8 Things You Need to Know
Doctors want to learn as much as possible about each person’s cancer and catch it early. That’s why, in some cases, they may recommend tumor marker testing during the various stages of diagnosis, treatment, and follow-up care. Tumor marker tests can provide important information about a cancer. Dublin heath screening looks at blood tests PSA for prostate cancer, CEA for bowel and lung cancer, Ca 15.3 for breast cancer, Ca 125 for ovarian cancer, Ca19.9 for pancreatic cancer. These are decided upon based on family history and medical risk assessment. These are processed at St James, Mater hospital and St Vincent’s Hospital Dublin 4 respectively, all through national centres of excellence.
- What are tumor markers?
Tumor markers are substances found in higher-than-normal levels in the blood, urine, or tissues of some people with cancer. These substances, which are also called biomarkers, can be made by the tumor. They can also be made by healthy cells in response to the tumor. Tumor marker tests check to see if you have these substances in your body and in what amounts. Tumor markers are often proteins. In addition, certain genetic changes are now being used as tumor markers. Our doctors have higher diplomas in dermatology to screen for skin cancers.
- Why are tumor marker tests used?
Along with other tests, tumor marker tests can help doctors diagnose cancer and recommend a treatment plan for an individual. Why, when, and how often these tests are done varies greatly from person to person. Rarely, they are used to help screen for a particular type of cancer in people with a high risk of the disease before they have signs and symptoms. But doctors mainly use tumor marker tests to predict how likely it is a cancer will come back after treatment and find it if it does
- Are there different types of tumor markers?
There are different types of tumor markers for different types of cancer. Certain tumor markers are associated with only one type of cancer. Other tumor markers are associated with more than one cancer. However, many cancers have no known tumor markers, so tumor marker testing may not be an option. Researchers continue to look for new and more effective tumor markers.
- What’s an example of how tumor marker testing can guide cancer care?
Understanding how tumor markers can affect your treatment choices can be complicated, but asking for examples can help. For instance, early-stage breast cancer has specific tumor markers that can help doctors tailor an individual’s treatment. If a person is diagnosed with this disease, the doctor may test for tumor markers known as estrogen receptor (ER) and progesterone receptor (PR). If the tests are positive for them, her doctor knows that the patient is more likely to be treated successfully with hormone therapy. If your doctor suggests tumor marker testing, ask which tumor markers you’ll be tested for and how often. Also, ask what the doctor hopes to learn from the testing.
- What are the limitations of tumor marker tests?
Tumor marker tests can provide a lot of helpful information, but they aren’t fail-safe. Just because a person has tumor markers, it doesn’t always mean cancer is present or has come back. Conditions besides cancer can raise tumor marker levels. Other limitations include: Tumor markers can go up and down over time, making it hard to measure them consistently. The level of a tumor maker may not go up until after the cancer is advanced. Some cancers don’t make tumor markers that can be found with current tests. Some people don’t have higher tumor marker levels even if the type of cancer they have usually makes tumor markers.
- How are tumor marker tests done?
There are three ways your doctor can test for tumor markers: a blood test. A member of our health care team will send a sample of your blood or urine into a laboratory for analysis. If a biopsy is done, a doctor will remove a small amount of tissue that will be examined by a pathologist under a microscope. You may need to repeat your tumor marker tests, because your tumor marker levels can change over time.
- What do I need to know about tumor marker test results?
There’s a chance that a tumor marker test can give a “false positive.” That means the results suggest a person has cancer or that the cancer is growing, even when it’s not. A tumor marker can also give a “false negative,” which means the results suggest a person doesn’t have cancer when they actually do. Or it can suggest a treatment is working when it’s not. That’s why other diagnostic tests are usually done along with tumor marker tests.
- Where can I learn more about tumor markers and tumor marker testing?
Ask your doctor to provide general information on tumor markers and tumor marker testing, as well as information specific to your type of cancer. You can also learn about tumor markers in the specific Type of Cancer sections on Cancer.Net.
Weight Reduction – How to Lose Weight
Lifestyle change for life
To lose weight and to keep it off, it is vital that you are motivated, really want to lose weight, and want to improve aspects of your lifestyle. Some people lose weight by strict dieting for a short period. However, as soon as the diet is over, they often go back to their old eating habits, and the weight goes straight back on. Losing weight, and then keeping it off, needs a whole change of attitude and lifestyle for life. This includes such things as:
- the type of foods and drink that you normally buy.
- the type of meals that you eat.
- your pattern of eating.
- the amount of physical activity that you do.
Top tip – ask family or friends to help and encourage you to keep to a healthy lifestyle.
Be realistic
What is your goal weight? Many people aim to get down to a ‘perfect’ weight. This is often unrealistic and may never be achieved. If the weight that you aim for is too low, you are likely to become fed up about slow progress, and give up. To lose 5 kg is good. To lose 10 kg is excellent. (10 kg is about one and a half stone.)
Top tip – in most cases, most health benefits come from losing the first 5-10% of your weight. This is often about 5-10 kg.
Timescale
What is your planned timetable? A weight reducing diet for about three months is realistic. After about three months, many people find it difficult to keep motivated. It may be useful to have a start and finish date for your weight-reducing diet.
It is best not to lose weight too fast. If you lose more than a kilogram per week, you may lose muscle tissue rather than fat. It is best to lose an average of ½-1 kg per week (about 1-2 lb per week). To do this you need to eat 500-1000 calories per day less than you did before your diet. You will lose 6-12 kg if you keep this up for three months. Don’t be disheartened by minor increases or levelling off in weight for a few days. Look for the overall trend over several months.
Top tip – aim to lose weight steadily for about three months.
Healthy eating and understanding food
Do you know which foods are the best to eat? In general, a healthy diet consists of foods high in starchy carbohydrates, fruits and vegetables, but low in fat, sugar, alcohol, and salt. Can you list several common foods that are in each category?
Top tip – low-fat foods are generally best. But remember, some low-fat foods and drinks are high in calories, such as alcohol, sugary drinks, and sweets.
Food diaries
It is helpful to know how much you normally eat. Estimating from memory is not very accurate. It is best to keep a diary, and write down every amount of food and drink that you have over a week or so. Include even the smallest of snacks. Add up the number of calories that you eat and drink each day. You may need advice from a practice nurse or dietician to calculate calories. However, there are plenty of books that give calorie counts for different foods.
It may be helpful to keep up the diary for several weeks to see the difference in calories that you eat before and after a change to a healthier diet. To lose weight, you must eat less calories each day than previously.
Top tip – do not forget the drinks. Some drinks contain lots of calories, such as alcoholic drinks and sugary drinks.
Planning what you eat
It is important to plan ahead. Perhaps you could plan each day’s meals and recipes the day before. In this way you will know exactly how much food you will be eating. This is better than looking in the cupboard and fridge before mealtimes or snacks to see what is there.
It is best to separate eating from other activities, as this helps to you keep to your planned eating for the day. So, try not to eat whilst on the move, whilst watching TV, during meetings, etc.
Top tip – plan tomorrows eating today.
Change of eating habits
Do you have any eating habits that can improve?
- Are you eating larger and larger portions when you have a meal? Try to deliberately take smaller portions when you have a meal. Do not feel that you have to ’empty your plate’. Perhaps change the plates that you have in your cupboard (which may be large) to more medium sized plates. In this way you will naturally serve up smaller portions.
- What do you have for snacks? Try changing chocolates or cakes for fruit.
- Do you have second helpings at meal times when you are really already full?
- Skipping meals is usually a bad idea. It sounds a good idea, but many people just become hungry, and have snacks later in the day, and eat too much at the next meal. Eating at regular mealtimes may be a first important change. Three healthy meals a day is best.
- Do you always have a pudding? Will a light yoghurt do instead of a sweet pastry?
- Do you eat quickly? Are you ready for a second helping before most people have half finished their first plateful? Obese people, on average, eat faster than non-obese people. It is best to train yourself to chew each mouthful for longer, and to eat slowly.
Top tip – three healthy meals each day, including breakfast, is better than skipping meals. Eat slowly, chew longer.
Shopping
One step towards improving eating habits is to change the contents of your shopping basket. For example, if you never buy biscuits, they will not be in the cupboard to tempt you. Most food labels say what is in the food, so it is easy to buy ‘healthy’ food. Some people argue that you should plan a shopping list, and stick to it. However, whilst you are learning which are the healthier foods, it may be better to spend some time comparing food labels before deciding on what to buy.
Top tip – do not shop for food when you are hungry. After a meal is best.
Recipes
Most people have a standard set of recipes and meals that they repeat. These may be old favourites, but may need to be abandoned in favour of new, healthier recipes. It takes time and effort to find recipes that you like.
Top tip – when you are on a weight reducing diet, try to learn a new ‘healthy’ recipe each week. When the weight reducing diet is over, you should then have plenty of new healthy meal ideas to help keep your weight down.
Drink mainly water
Many people use drinks full of calories to quench their thirst. Sugary drinks such as cola, tea and coffee with milk and sugar, milk, and alcoholic drinks, all contain calories. One of the easiest ways to cut back on calories is simply to drink water as your main drink.
Top tip – keep some water in a plastic bottle in the fridge. Chilled water is surprisingly refreshing.
Physical activity
If you are able, aim to do at least 60-90 minutes of moderate physical activity on at least five days a week. (All adults should aim for at least 30 minutes on five days a week. However, 60-90 minutes is recommended if you are overweight or obese and are aiming to lose weight.) Moderate physical activity includes: brisk walking, jogging, dancing, swimming, badminton, tennis, etc. In addition, try to do more in your daily routines.
Top tip – If you are not used to physical activity, try starting with a 30 minute brisk walk every day and then building up from there.
Morale
The first kilogram is the easiest to lose. This is because you lose water from your body at first as well as fat. Be aware that the first kilogram or so may seem to fall off, but then the weight loss slows down. This is normal, so don’t get disheartened!
Top tip – regular weighing and encouragement by a practice nurse or dietician is often helpful.
Special diets
Special ‘wonder’ diets are often advertised, but they are often not helpful. This is because your old eating habits will usually return after a short ‘special diet’, and weight often goes back on.
Top tip – it is not usually a special diet that you need, but a life-long change to a healthy diet.
Tempting situations and special occasions
It is important to recognise that holidays, festivals, eating out, etc, may interfere with your everyday food choices and eating schedule. Also, do you find that watching food programmes on TV makes you hungry? How about smells from the kitchen from someone cooking who is not aware that you are trying to lose weight? Do you get pressure from family or friends to eat or drink more?
You will be tempted by different situations to abandon your planned food intake. Can you identify any tempting situations? Can you avoid them? If not, how do you cope with them?
Top tip – go and clean your teeth when you are tempted to eat between meals.
Stress and depression
Many people eat as a comfort, or as a way of coping with stress. How do you cope with stress? Is stress, unhappiness, depression, etc, a reason for you to overeat or to binge eat? If so, can you plan alternative strategies. For example, relaxation tapes, going for a walk, talking to a friend, etc.
Top tip – see a doctor if you feel that depression is a problem. Depression can often be treated.
The power of the appetite
The appetite is a very powerful feeling. This is why many people find it so difficult to lose weight. There is no easy answer to this. Some people feel hungry more often than others. Feeling hungry does not always mean the body needs food. You have to be aware of the power of your appetite, and try to resist eating as soon as you feel hungry. One way of helping with a strong appetite is to fill up at meal times with vegetables and fruit which have a lot of fibre and bulk, but are low in calories.
Top tip – drink lots or water, and eat lots of fruit and vegetables to help counter appetite.
Medical treatments
- Medicines to help with weight loss are an option in some cases. They may help, but they are not wonder-drugs, and you still need to eat less. Doctors are given guidelines on when to prescribe these medicines.
- Counselling or referral to a dietician for advice is sometimes useful, but may not be available in all areas. Counselling may be done ‘one-to-one’, or in a group setting.
- Surgery is an option if you are very obese. Results are usually good, but surgery is not without some risk. And, you still have to reduce the amount that you eat afterwards.
Keeping to a reduced weight
Many people who lose weight soon put it back on again when they stop their weight reducing diet. The main reason this happens is because the weight reducing diet was only a temporary cut back of an unhealthy diet. Once you have lost some weight, to keep the weight off you need to stick to a healthy diet. An active lifestyle with more physical activity would also help. Even better is for the whole family or household to have changed to healthy eating habits and a healthy lifestyle.
To keep your weight down you will still need to eat less and/or do more physical actvity than previously. For example, if you have lost 10kg, to keep this off and maintain your weight you will still need to:
- Eat about 300 calories per day less than you did prior to the weight loss diet, or
- Do more physical activity to ‘burn up’ an extra 300 calories per day, or
- A combination of the two.
Top tip – after losing some weight, weigh yourself once a week to keep a check on your weight.
Body mass index
Your body mass index (BMI) is a good estimate of how much of your body is made up of fat. It relates your weight to your height. You can work out your BMI by dividing your weight (in kilograms) by the square of your height (in metres).
So, for example, if you weigh 70 kg and are 1.75 metres tall, your BMI is 70 / 1.75 x 1.75, which is 22.9. Alternatively, your practice nurse can measure and weigh you, and tell you your BMI.
| BMI | Classed As | Health Risk |
| Less than 18.5 | Underweight | Some health risk |
| 18.5 to 24.9 | Ideal | Normal |
| 25 to 29.9 | Overweight | Moderate health risk |
| 30 to 39.9 | Obese | High health risk |
| 40 and over | Very obese | Very high health risk |
MSU (Mid-stream Specimen of Urine) at Dublin health Screening
 What is the purpose of an MSU test?
What is the purpose of an MSU test?
- To confirm the diagnosis of a urine infection. The usual symptoms of a urine infection are pain when you pass urine, and passing urine frequently. However, symptoms are not always typical, particularly in children and the elderly, and a urine test is needed.
- To decide the best antibiotic to use. Some bacteria (germs) are resistant to some antibiotics. If the test shows that bacteria are in the urine then the bacteria are tested against various antibiotics. This finds which antibiotics will kill the bacteria in the urine.
How do I do a mid-stream specimen of urine?
The aim is to get a specimen (sample) of urine from the middle of your bladder. Urine is normally sterile (no bacteria present). If bacteria are found in the sample, it means that the urine is infected. A ‘mid-stream’ sample is best as the first bit of urine that you pass may be contaminated with bacteria from the skin.
Women – hold open your labia (entrance to the vagina). Men – pull back your foreskin. Pass some urine into the toilet. Then, without stopping the flow of urine, catch some urine in a sterile bottle. (The bottle is usually provided by a doctor or nurse.) Once you have enough urine in the bottle, finish off passing the rest of your urine into the toilet.
Do not open the sterile bottle until you are ready to take the sample. You do not need to fill the bottle to the top, a small amount will do. (Some specimen bottles contain a preservative. If this is the case, a mark on the bottle will indicate the ideal amount of urine. However, if that is difficult, any amount is better than none.)
Haematuria
- Positive test indicates either haematuria, haemoglobinuria or myoglobinuria.
- Dipstick test for presence of haemoglobin with degree of colour change directly related to amount present.
- Can appear as both coloured dots and change in the colour field.
- False positive readings are most often due to contamination with menstrual blood. Incidence of false positives can be increased by dehydration which concentrates the number of RBCs produced and exercise.
- Haematuria is defined as >3 RBC/high power field (hpf) of centrifuged sediment under microscope.
- Dipsticks are 90% sensitive but somewhat less specific.
- Prognostic significance of positive test is very controversial, rates ranging from 0.5 – 6% of patients with positive test have been found to have underlying significant pathology.
Proteinuria
- Healthy adults normally excrete 80-150mg protein in urine daily.
- Detectible proteinuria may be first sign of renovascular, glomerular or tubulo interstitial renal disease.
- Alternatively may be caused by overflow of abnormal proteins in diseases such as multiple myeloma.
- The dipstick detects presence of protein by increasingly darker shades of green. Minimum detectible protein concentration is 20-30mg/dl.
- False negatives can occur in alkaline or dilute urine or when primary protein is not albumin. More accurate method is to precipitate urinary proteins with 3% sulfosalicylic acid (detects at 15mg/dl and detects other proteins). If urine negative on dipstick but strongly positive with sulfosalicylic acid, suspect multiple myeloma. With positive test use quantitative 24 hour urinary collection and test with protein electrophoresis or immunoassay.
Proteinuria
- Transient; occurs commonly especially in children and usually resolves within a few days often associated with fever, exercise or stress. In older patients may be due to congestive heart failure.
- Intermittent; frequently associated with postural changes. Commonly occurs in upright position in young adults and rarely exceeds 1g/day. Resolves spontaneously in about half of patients and not associated with disease. If normal renal function evaluate no further.
- Persistent; usually due to glomerular cause with >2g protein/day of which major component is albumin. Some may also coexist with haematuria.
Glucose
- Useful screen for diabetes mellitus.
- Urine testing for glucose is also useful in patients who find blood glucose monitoring difficult. Tests for glucose range from reagent strips specific for glucose to reagent tablets which detect all reducing sugars. Tests for ketones by patients are rarely required unless they become unwell.
- Nearly all glucose filtered by the glomeruli is reabsorbed in the proximal tubules and only undetectable amounts appear in urine in healthy patients. Above renal threshold (180mg/dl) glucose will appear in urine. Test relies upon reaction of glucose with glucose oxidase on dipstick to form hydrogen peroxide which causes colour change. This is specific to glucose and no other sugar.
Ketones
- Occurs in diabetic ketoacidosis, pregnancy and following starvation or rapid weight loss.
- Dipstick test presence of aceoacetic acid at 5-10mg/dl but not acetone or beta-hydroxybutyric acid.
Bilirubin and urobilinogen
- Urine normally contains no bilirubin and only very little urobilinogen.
- Conjugated bilirubin only appears in urine in presence of liver disease or obstruction of bile duct.
Leucocyte esterase and nitrite test
- Leucocyte esterase activity is due to presence of white blood cells in urine.
- Nitrites strongly suggest bacteriuria. They are present because many species of gram-negative bacteria convert nitrates to nitrites.
- Test has variable sensitivity but high specificity. May not be a suitable substitute for microscopic examination.
Note a macro analysis of the urine sample is carried out in the practice and the sample is also sent to St James or St Vincents for culture and sensitivity.
Full STD Screen (optional)
Dublin health Screening is linked via the National Health Link project to the labs of St Vincents Hospital and St. James directly to ensure rapid results. Note a full STD screen at our Fitzwilliam street office in Dublin 2 is 125 euro and this includes the consultation rate and transfer of all samples to the national viral reference lab in UCD.
In the last 7 months we have seen a rise in the number of cases of chlamydia in the Dublin area. This is very important as it can often have no symptoms and yet can go on to cause pelvic inflammatory disease in women and hence later lead to infertility. There are a number of reasons for this including changes to the social demographic and there has also been a high incidence seen in the student population.
What is an STI?
A sexually transmitted infection (STI) is an infection that can be passed from person to person when having sex. You can get an STI by having vaginal sex, anal sex, or oral sex. There are several different types of STI.
What are the main STIs?
The ten most common STIs in the Ireland are: anogenital warts, chlamydia, genital herpes, gonorrhoea, HIV, hepatitis B, hepatitis C, pubic lice, syphilis, and trichomonas. These are briefly described below.
Anogenital wartsare small lumps that develop on the genitals and/or around the anus (back passage). They are sometimes just called genital warts. They are caused by a virus called the human papillomavirus (HPV). However, most people infected with HPV do not develop visible warts. You can be a ‘carrier’ of the virus without realising it, and you may pass on the virus to others who then develop warts. Treatment options include applying chemicals to the warts or freezing the warts to destroy them.
Chlamydia is caused by a bacterium (germ) called Chlamydia trachomatis. It is the most common STI in the Ireland. Symptoms include a vaginal discharge in women, and a discharge from the penis in men. You can be infected with chlamydia for months, even years, without realising it as it often causes no symptoms. However, even if you have no symptoms, you can still pass on the infection and complications may develop if it is left untreated (such as pelvic infection and infertility in women). A short course of an antibiotic clears chlamydia in most cases.
Genital herpes is caused by the herpes simplex virus. Once you catch this virus it stays with you for life but lies dormant without causing symptoms for most of the time. In fact, many people who are infected with this virus never have symptoms. If symptoms occur, they can range from a mild soreness to many painful blisters on the vulva or penis and surrounding area. A first episode of symptoms can last 2-3 weeks, but may be shorter. Recurrent episodes of symptoms then develop in some cases from time to time, but are usually less severe than the first episode. (It is similar to having ‘cold sores’ on the genitals from time to time.) Antiviral medication can ease symptoms when they develop
Gonorrhoea is caused by a bacterium called Neisseria gonorrhoeae. Symptoms include a vaginal discharge in women, and a discharge from the penis in men. Again, some people infected with gonorrhoea do not develop symptoms. However, even if you have no symptoms, you can still pass on the infection and complications may develop if it is left untreated (such as pelvic infection and infertility in women). A short course of an antibiotic clears gonorrhoea in most cases.
HIV (human immunodeficiency virus) is most commonly passed on by sexual contact. HIV attacks cells of the immune system. Over time (usually several years) the immune system ‘weakens’ so that you cannot defend your body against various bacteria, viruses and other germs. This is when AIDS develops (acquired immunodeficiency syndrome). Many infections and conditions can develop if you have AIDS. Treatment with antiretroviral drugs can reduce the ‘viral load’ of HIV and allow your immune system to work effectively. However, treatment does not clear the virus from the body. Therefore, if you are infected with HIV you will need monitoring for the rest of your life, and treatment is long-term.
Hepatitis B is a virus that primarily attacks the liver. The virus is mainly passed on by sexual contact, sharing contaminated needles to inject ‘street drugs’, or from an infected mother to her baby. The hepatitis B virus can cause a short term (acute) infection, which may or may not cause symptoms. Following an acute infection, some people develop a persistent infection called chronic hepatitis B. Many people with chronic hepatitis B remain well, but can still pass on the virus to others (as they are ‘carriers’). Some develop serious liver problems. If needed, antiviral medication may prevent or reduce the severity of liver inflammation and liver damage.
Hepatitis C is is a virus that primarily attacks the liver. Most cases occur in people who share needles to inject ‘street drugs’ that are contaminated with traces of infected blood. There is a small risk that an infected person can pass on the virus whilst having sex. Some people clear the infection naturally. Some people with persistent infection remain free of symptoms, but some have symptoms. After many years of infection some people develop cirrhosis (a severe scarring of the liver), and some develop liver cancer. Treatment is difficult but it can clear the infection in up to half of cases.
Pubic lice(often called ‘crabs’) are tiny insects about 1-2 mm long (smaller than a match-head). They lay eggs which hatch into lice after seven days. Pubic lice attach strongly to hairs, and do not wash or brush off with normal cleaning. Pubic lice are passed on by close bodily contact, especially when having sex. The main symptom is itch, usually in the pubic hair area. However, you may not have any symptoms, but may still pass on the lice to others. Treatment with a lotion or cream usually clears the lice.
Syphilis is caused by a bacterium called Treponema pallidum. If it is not treated, it can spread in the bloodstream from the genital region to cause various symptoms and problems in different parts of the body over many years. A short course of antibiotics usually clears syphilis infection.
Trichomonas is a protozoan, which is a tiny germ similar to bacteria. It can cause an infection that is not normally serious but symptoms can be unpleasant. Symptoms include a vaginal discharge in women, and a discharge from the penis in men. Some people infected with trichomonas do not have symptoms but can still pass on the infection. A course of antibiotics usually clears trichomonas infection.
There are some other STIs that are uncommon in Ireland. For example, donovanosis and chancroid.
Sexually transmitted infections are common. Remember any sexually active person may be exposed to a sexually transmitted infection. If you suspect you have an infection get it checked out as soon as possible. Most treatments are simple and painless and you do not have to be admitted to hospital. Treatment is confidential, non judgmental. The staff in the clinic are trained to treat sexually transmitted infections in an understanding and helpful way so there is no need for you to feel embarrassed. If you are pregnant and think you may have picked up a sexually transmitted infection it is particularly important to get it checked out and treated as soon as possible. The D2 medical centre in Dublin 2 provides a private, comprehensive Sexually Transmitted Infection service which includes full STI testing, advice and necessary referrals or prescriptions.
A full physical examination is a general examination of the body performed by the doctor or general practitioner (GP). The examination will cover most of the basic systems of the body, including the heart system, lung system, gut system and nerve system examination. Additional examination can be added depending on the clinical scenarios. The purposes of a full physical examination is to confirm any present issues after the clinical history; and to find possible pathologies that are present but yet to be known about.
Full Physical Examination (A Check-Up) at Dublin health screenClinical history and physical examination are the essential part of medicine since Western medicine was established centuries ago. However with the advance of technological investigations, many diseases are diagnosed with blood tests and imaging studies. Many diseases are diagnosed earlier using modern technology where previously physical examination could find nothing, for example prostate cancer, colon cancer, etc.
Before a physical examination is carried out, the doctor will ask for consent from the patient. If the patient is of a different gender from the doctor, a chaperone may be needed (especially when a male doctor examines a female patient). Usually some parts of the body will need to be exposed, and permission is obtained as well.
The physical examination usually starts with the vital signs, and that include the heart rate, blood pressure, respiratory rate and temperature.
Generally, there are 4 parts of physical examination:
- Inspection: looking for signs
Palpation: feeling for signs
Percussion: tapping for signs, used when doing a lung and/or gut examination.
Auscultation: listening using the stethoscope, or in olden times, purely listening with direct ear.
Depending on the doctor, the sequence of the systems covered may be different. However all physical examinations strive to determine more about the present disease the patient has, or possible diseases that are yet to be diagnosed.
During the physical examination, the doctor strives to keep the patient as comfortable as possible. However, sometimes tender spots need to be touched and examined for accurate or reliable diagnosis.
After the physical examination, the patient will be asked to dress, and then the doctor will tell the patient the clinical findings.
Complications:
Aside from some discomfort for some patients, physical examination has no severe risks usually.
Screening:
Because physical examination is low cost (only the cost of expertise is needed), non-invasive (ie. not entering the body cavity in any way) and potentially revealing, they are recommended as screening tests for certain diseases such as breast cancer, skin cancer and even prostate cancer. These screening tests need to be done in conjunction with the patient’s respective clinical histories, hence they need to be discussed with the doctor.